Digest
WHERE CAN RADIOLOGY
GO WRONG?

in your Food
FREE TO DISTRIBUTE
BROUGHT TO YOU BY
CAPPTOO AG
FREE TO DISTRIBUTE
BROUGHT TO YOU BY
CAPPTOO AG

BY SIMON SPICHAK


BY SIMON SPICHAK

If an AI for pulmonary scans was trained entirely on patients from the northeast US, and now encounters cases from the southeast US, its performance worsens. The AI algorithm starts to see a lot of pulmonary nodules in the southeast and might begin to classify almost everyone down there as having cancer. It will not realize that the nodules are common and caused by endemic fungi.
Perchik:
The AIs are used for flagging things like pulmonary nodules and breast masses. So, it’s very limited right now. We had our AI boom about one or about two years ago, and we still are having, you know, dozens and dozens of new applications getting FDA clearance, but they’re going for these same targets. High-volume, high-acuity studies for targeted cancer applications have not been as highly researched.
Perchik:
The most important thing is fundamental knowledge of
how the AI works. This means understanding what type of data the AI uses and how well this was trained. Was it challenged with a lot of external data? Or was the AI developed in a single institution?
Those kinds of single-institution tools are the most brittle and
might perform worse if challenged with new types of data. Beyond that, knowing how to roll AI out in
a regimented, meticulous way is important. This isn’t like buying a new X-ray machine; it won’t work right out of the box. You have to test it. You have to have feedback; you have to have a close relationship with the vendor. You have to be more meticulous, and you have to monitor its performance over time.

Zahra’s life took a sharp turn in January 2021 when she was diagnosed with breast cancer. While changing clothes, she randomly examined her body and found a lump in her left breast. As was rightly put by Zahra, “The second you accept that you have it and accept that you will suffer from side effects of the treatment process, the easier it is to go through these things.”
Globally, female breast cancer has surpassed lung cancer as the most commonly diagnosed cancer. According to the World Health Organization, in 2020, around 2.3 million women were diagnosed with breast cancer worldwide, and 685,000 died of it. In Pakistan, the stats are not any different. Annually, around 40’000 women die of breast cancer in Pakistan, with an additional 90,000 being diagnosed with the disease.
World Health Organization (2020, 2023)
“It didn’t feel like the end of the world, but I certainly cried. It was shocking, but not like I was in a complete state of shock.” Being a Muslim, she said breast cancer strengthened her faith in Allah. “I believe that Allah makes you go through everything for a reason. During cancer, my baking business went up exponentially, so much so that I had to leave my job,” she added. “Allah compensated me.”
The benefit of mammograms in detecting breast cancer early and saving women’s lives is clear, as Zahra’s experience illustrates. However, many women in Pakistan, a predominantly Muslim country, do not even bother to go through the annual procedure. Some women even believe that God controls diseases and cures.
A study involving 1,000 women analyzed knowledge, attitude, and practice (KAP) regarding breast cancer among Pakistani women and found that only 32% of the participants had proper awareness regarding the disease process, the purpose of mammography, and breast cancer prevention, and only 19.6% of them had undergone mammographic screening. Another study published in “BMC Women” explored the barriers that hinder women in Pakistan from seeking timely screening and treatment. The study found lack of awareness, hesitance in accepting social support, spiritual healing, feminine sensitivity, stigmatization, aversion to male doctors, lack of financial resources, and apathetic medical services as some of the barriers that hinder screening and treatment.
Modesty is a significant factor that influences Muslim women’s health decision-making. Adherence to religious teaching in covering the aurah (the intimate parts of body) caused some Muslim women to be concerned about having close physical contact and exposing their body parts to others of the opposite gender.
Worrying about maintaining modesty during a mammogram is one reason some respondents do not want to have one. Studies reported that some Muslim women were concerned with the altered image of losing their breasts and becoming less attractive and feminine if diagnosed with breast cancer. This is because, culturally, women’s breasts are associated with motherhood, feminity, and sexual desire.
“People are ashamed of breast cancer, which one should not be as no one goes through it with her own will,” said Zahra. Pakistan is ranked amongst the emerging and growth-leading economies, it is not progressive in the way its society addresses this issue.
While discussing her journey with our magazine, Zahra talked about one of her acquaintances who was in her 80s when she was diagnosed with breast cancer. Due to cultural constraints, she refused to go through a mastectomy after chemo sessions and got the disease back after five years. “Women are not putting themselves first; they are putting society first.”

Zahra got her treatment done at Aga Khan University Hospital, one of the top tertiary care hospitals in Karachi, Pakistan. Since Zahra was diagnosed with stage 2, grade 3, triple-negative breast cancer, an aggressive type, the doctors acted quickly. She underwent 16 chemotherapy sessions, a double mastectomy, and 19 radiotherapy sessions. As of now, she is cancer- free.
According to Zahra, faith helped her throughout her treatment journey. “My journey brought me closer to Allah. It was faith that got me where I am today, that got me through my journey quickly and easily.”
“I found the CT scan very scary, and I was constantly reciting Surah Fatiha; I was praying to Allah that my cancer had not spread. When Ihadthedyeinme,Ididnot overthink anything and underwent the procedure in the dark. I did not ask anyone about their experiences, which calmed me. When the dye was in me, I did not feel anything.”
After the CT scan, a bone scan was conducted to see if the cancer had spread to the bones, which was another horrible experience for Zahra. “I was constantly reciting duas (Islamic chants) the whole time, which helped me through it.”
Zahra went through psychotherapy night before her first chemo session, which she found very helpful. “That set up the tone of my journey, and the next day, I woke up for my chemo and went in like a boss.”
Since breasts constitute a main part of femininity for women, mastectomy is the hardest decision for women with breast cancer. So, as for Zahra, she had second thoughts about keeping one breast to breastfeed her child whenever she had one.
Here, her husband tried convincing her, saying, “Do not risk your life for someone who does not even exist yet.” Hence, she put her life first and underwent a double mastectomy. Had she decided to keep her other breast, the likelihood of getting cancer back would be much higher.
Apart from that, Zahra talked about the effects of chemotherapy, like losing hair and energy. “Losing hair on my head was fine for me. I was prepared for it. It did not hit me hard. But losing my eyebrows was everything. I wanted to keep them, so I would buy eyebrow tattoos from Daraz (an e-commerce platform).”
While going out, people could barely tell that she had cancer, as she used to cover her head when going out. “Sometimes I would go out completely bald, and there one beggar asked me why I was bald, and I boldly replied, I’ve got cancer.”
When asked about the effects of the treatment she experienced, Zahra said, “It affects me now. During treatment, I was a crazy warrior, but now that treatment is over, I’ve had trouble sleeping and do have epiphanies like, Oh my God, they are gone. A woman is supposed to look a certain way; that is what we are constantly taught. And once that is gone, what are you going to do? There are options for reconstruction, which I do not want to go for right now as it causes much pain.”

Since Zahra was quite young, the doctor had to see if the cancer was genetic. Although she has strong genes of cancer from the paternal side, she was told that cancer passed down from the maternal side, so they are all clear, which was a myth.
As she continued to hold talks for breast cancer awareness, she tells Digest about myths around breast cancer in Pakistan, which included that cancer being contagious and radiation from microwaves or wearing a black bra may cause cancer.
A study highlighted myths and misconceptions about breast cancer in the Pakistani population. Some common myths include that breastfeeding offers immunity to breast cancer, breast cancer spreads after biopsy, faith healers and alternative medicine can cure breast cancer, and only painful lumps are associated with breast cancer. Some participants also believed breast cancer resulted from God’s curse or evil eye.
The fear, stigma and shame associated with cancer within Pakistan hold people back from talking about their experiences, going for screenings, and even treatment. Zahra says: “People would be talking to me about my health and used to mute breast from the conversation, which offended me. It’s a Pakistani cultural thing.”
Men leave their wives when they find out they have cancer. People fear their daughters won’t get married if someone in the family has/had cancer, and the male family members will not support them or stick around. Zahra had married the love of her life in 2018. Life with Babar was perfect, they run a thriving baking business.
“My friends tell me it’s remarkable that your husband is there for you. I know that it is coming from somewhere, as they have seen men leaving their wives for having cancer. When I was undergoing radiation therapy, one lady asked if my husband would allow me
to undergo surgery. I could not comprehend the question.”
“The first thing on my mind was how I would pay for this. I did not realize I had a corporate job and health insurance. My husband has health insurance for his spouse. My company was very supportive throughout my treatment. They bumped up my insurance.”
The average annual income in Pakistan is about 150 Euros. The treatment cost may range from as little as 300,000 to over 2 million Pakistani rupees (7000 Euros). The most basic form of chemotherapy for one patient can cost as much as 60,000 to 80,000 rupees, so early detection can reduce costs. Given that there is no health insurance for common citizens in Pakistan, many breast cancer patients cannot afford the treatment cost and benefit from the welfare.
Shaukat Khanum Memorial Trust, Bait-ul-Sukoon Cancer Hospital, Indus Hospital, and Kiran Cancer Hospital are some of the best cancer hospitals in Pakistan that use state-of-the-art facilities and are established to meet the growing demand of poor, deserving cancer patients free of charge.
According to Zahra, who got her treatment at Aga Khan University Hospital, western hospitals have better facilities and rooms. They have a tradition of ringing a bell to celebrate the end of chemotherapy sessions. Hospitals abroad have a better quality of treatment, not in terms of medicines but in terms of taking extra care of their patients, which Pakistan lacks.
She also pointed out the lack of healthcare resources in Pakistan: “We don’t have enough oncologists and breast surgeons. Government figures have revealed that less than 250 individuals have qualified in the country as trained medical or radiation oncologists, and the country has 27 cancer treatment centers, a figure experts deem insufficient given the high number of cancer patients.”

While answering whether one should go for treatment in Pakistan or abroad, she said, “Do it where your support system is because you need your family and your friends around you throughout your journey; that is very important for recovery. It is nice to have your doorbell rung with a bouquet of flowers daily.”
For a Muslim country like Pakistan, visiting the sick for a short while is part of Sunnah. Even if physical visits are not possible, family and friends should maintain connection via phone calls, WhatsApp, or other ways to stay in touch.
She emphasized that while some people are afraid upon hearing about a cancer diagnosis and disappear, they must face up to this and offer support.
While advising people who have cancer, Zahra stressed the importance of adhering to the treatment being recommended by their doctor. She said, “Know what you have got to do to beat it and make sure you do all of it. Cancer treatment is so difficult that you do not want to go through it again.”
From the Islamic perspective, there are some positive aspects of illness in general and breast cancer in particular, as it gives Muslims the opportunity to assess, reassess, and think deeply about life here and whether or not they are walking on the path that will find them the solace in this world and the other world. “My life is better after cancer because it has opened up my mind.”



“I’m convinced epidemiology can change the world if we think about cancer more holistically.”
Prof. Prisco Piscitelli



Example of food with high nutritional value
Photo source: Unsplash; author: Reka Biro-Horvath


ONCOLOGY COMPASS IS GLOBALLY BECOMING AN INCREASINGLY IMPORTANT PLATFORM FOR ONCOLOGISTS

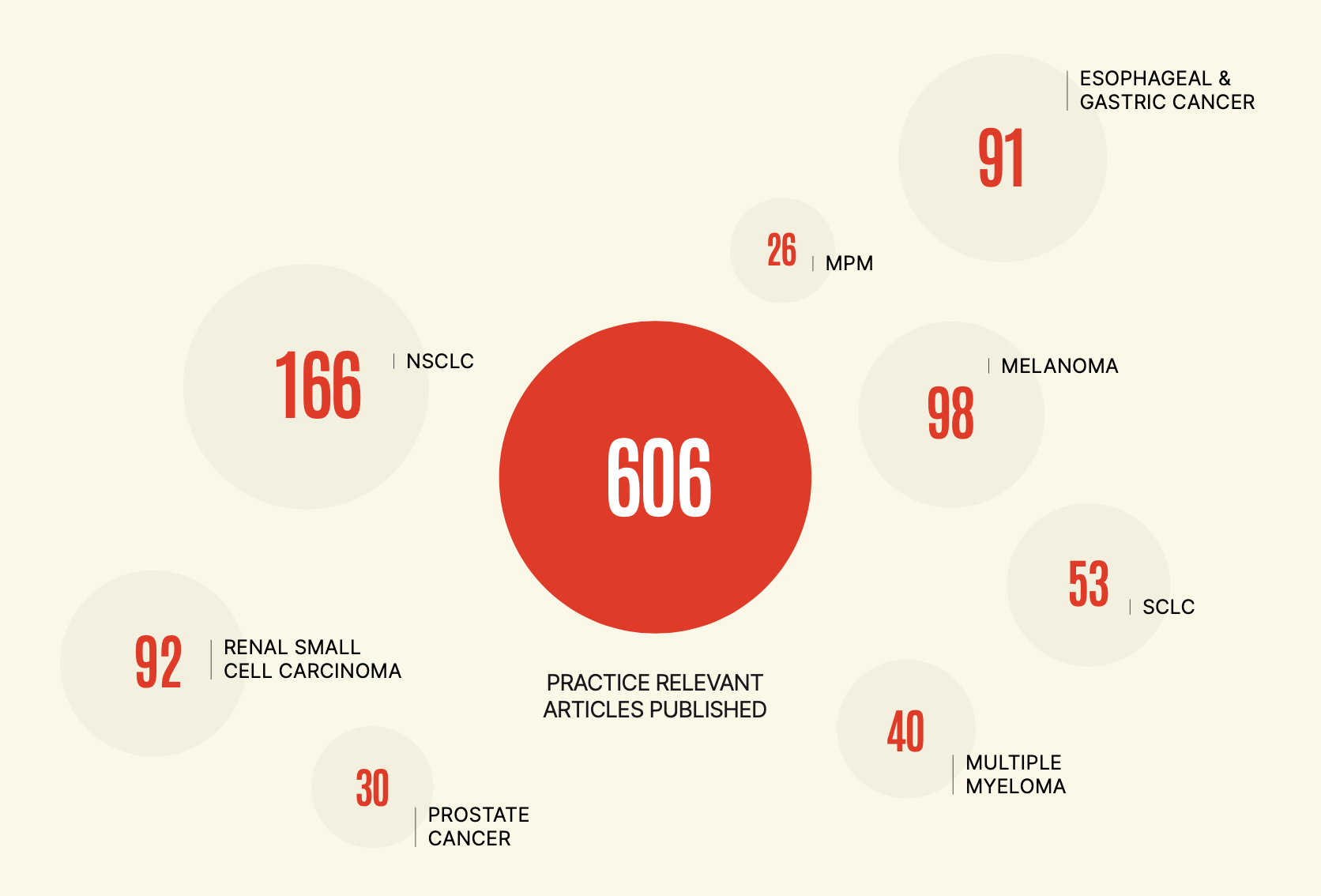
308
ACTIVE
users
TOP 3 FILTER
CRITERIA:
RCC
MELANOMA
NSCLC
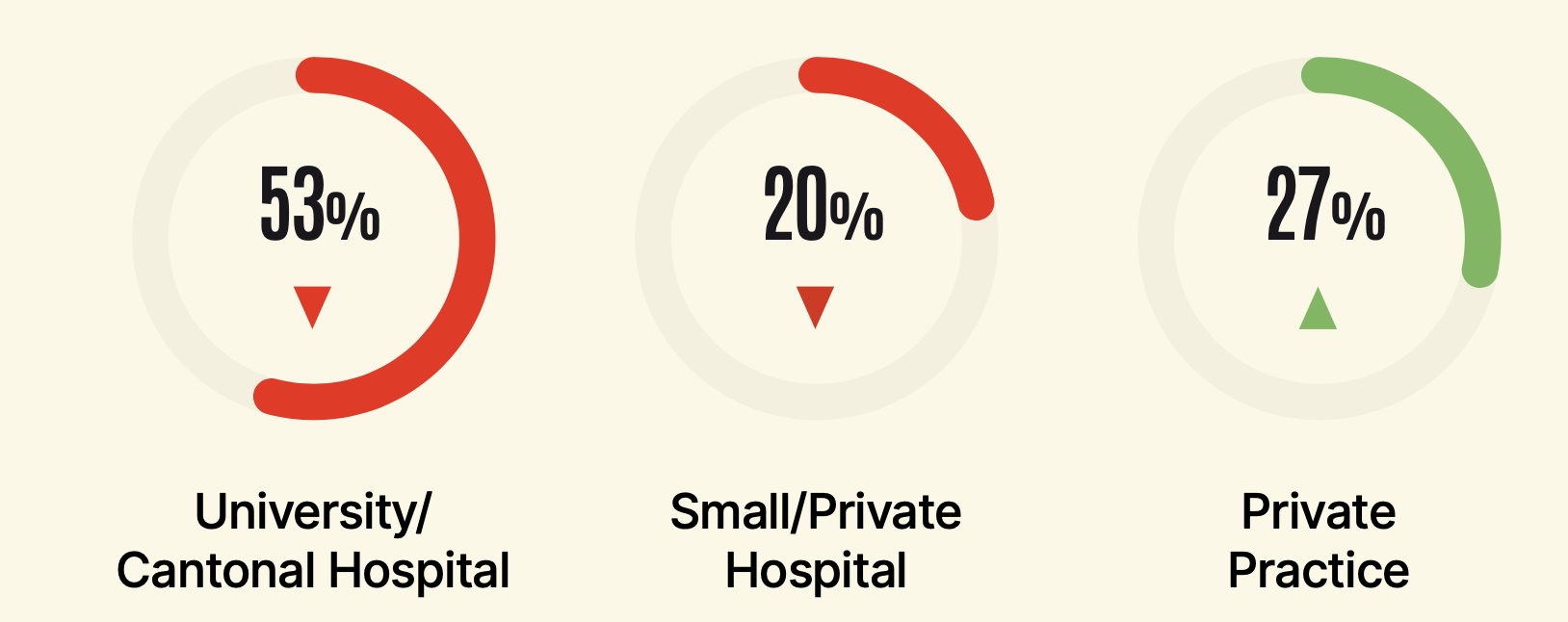
The Digest for the Oncologists is edited and hosted by Capptoo AG, incorporated in Zürich, Switzerland.